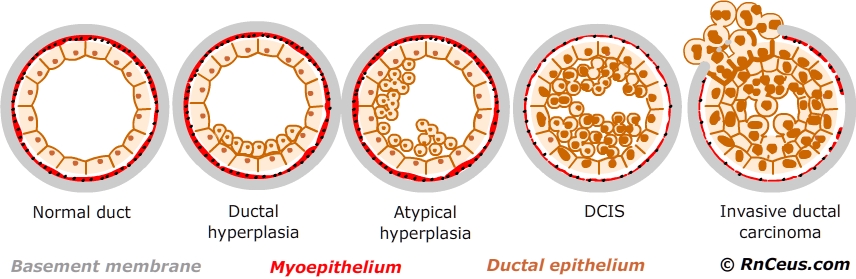
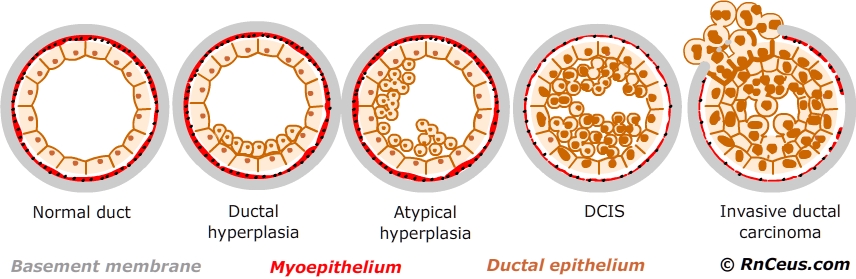
Ductal carcinoma in situ (DCIS) is one of several epithelial proliferative breast diseases which include: epithelial hyperplasia, atypical ductal hyperplasia (ADH), DCIS and invasive ductal carcinoma (IDC). Ductal epithelial hyperplasia without atypia confers only a slight risk of progression to IDC, about 1.5-2x greater risk then normal ductal epithelium. Atypical ductal hyperplasia confers a moderate risk of progression to IDC, about 4-5 times greater than normal ductal epithelium. DCIS (low grade) increases the risk of progression to IDC about 8-10 times normal. A very high risk, ≈ 50% of recurrence or IDC is associated with high grade DCIS.
Over time several systems have been created to differentiate DCIS from hyperplasia and help categorize the risk posed by a particular DCIS lesion.
Chapman, et el. (2007) state nuclear grading is an important component of medical treatment decisions for DCIS. There are three grades of DCIS currently described.
Grade I – low or no grade – DCIS cells look similar to normal or atypical ductal hyperplasia cells.
Grade II – moderate or grade – DCIS cells grow faster than normal cells and look less like them.
Grade III – DCIS cells tend to grow more quickly looking less like normal breast cells. Often described as comedo or comedo necrosis which refers to areas of dead (necrotic) cancer cells.
 |
 |
 |
 |
 |
 |
Growth patterns and architectural classification was the earliest attempts to classify DCIS lesions. The following architectural patterns are listed from least aggressive to most aggressive forms:
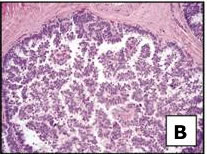
A. Papillary pattern: Characterized by fern-like processes within the duct. Cells are arranged around fibrovascular cores
B. Micropapillary pattern: Characterized by small tufts of cells within the duct. The tufts lack fibrovascular cores present in papillary forms. Cells are small to medium in size, and the nuclei show diffuse hyperchromasia; mitoses are infrequent.
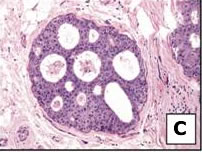
C. Cribriform pattern: Characterized by fenestrations between cells. Cells are smaller and more uniform compared to comedo pattern. This pattern may also be present in comedo DCIS.
D. Solid pattern: Characterized by a lack of significant necrosis, fenestrations, or papillae. Cells may be large medium or small, they fill and distend the duct.
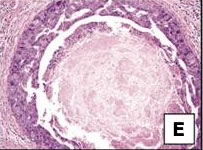
E. Comedo pattern: Characterized by prominent central necrosis. The necrotic material often becomes calcified, enhancing detection on mammogram. Calcified "casts" may be linear, branching or granular. Cells are large with nuclear pleomorphism. Mitotic activity is often elevated.
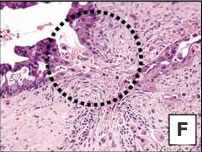
F. Invasive ductal carcinoma: Characterized by erosion through the basement membrane and migration of abnormal cells into the surrounding tissue.
Architecture and growth patterns are still included in the pathology report but their clinical relevance is suspect for many reasons:
Instant Feedback:
Both DCIS and LCIS are characterized by erosion through the basement membrane and migration of abnormal cells into the surrounding tissue.
Nuclear grading of DCIS has greater predictive value then architectural pattern alone.
- Low grade (Grade I) - monomorphic nuclei (well differentiated)
- nucleus size ≈ 1.5X to 2.0X RBC diameter or = to a normal duct epithelial cell nucleus
- finely dispersed chromatin
- occasional nucleoli
- occasional mitoses
- nuclei polarized toward the luminal space.
- often estrogen receptor (ER) and progesterone receptor (PR) rich
- intermediated nuclear shape
- intermediate size
- intermediate chromatin dispersal
- intermediate nucleoli
- intermediate mitoses
- intermediate polarization of nuclei
- nucleus size >2.5X RBC or a normal duct epithelial cell nucleus
- vesicular and irregular chromatin distribution
- nucleoli are prominent and often multiple
- mitoses may be frequent
- nuclei usually not polarized toward the luminal space
- associated with increased risk of local recurrence
- often estrogen receptor (ER) and progesterone receptor (PR) poor
Pleomorphic LCIS is characterized by
- marked nuclear pleomorphism (at least a 2- to 3-fold variation in nuclear size),
- nuclear membrane irregularity, and variably prominent nucleoli
- Mitoses can be seen and may be numerous.
- Central necrosis with associated calcifications is frequently present.
References:
Chapman, J. W., Miller, N. A., Lickley, A. Qian, J. Christens-Barry, W. A., Fu, Y., et al. (2007). Ductal carcinoma in situ of the breast (DCIS) with heterogeneity of nuclear grade: prognostic effects of quantitative nuclear assessment. BMC Cancer. 7, 174.
Kim, J., Moon, H., et al. (2012). Prognostic and Predictive Factors: Prognostic Factors - Clinical The grade of accompanying DCIS in IDC as important prognostic factor. The Journal of Cancer Research. 72(24),10-35.
Lester, S., Bose, S., et al. (2009). Protocol for the Examination of Specimens from Patients With Ductal Carcinoma In Situ of the Breast. Archives of Pathology & Laboratory Medicine. 133, (1), 15-25.
Scoggins, M., Krishnamurthy, S., Santiago, L. & Yang, W. (2013). Lobular carcinoma in situ of the breast: clinical, radiological, and pathological correlation. Acad Radiol. 20(4),463-70.
© RnCeus.com